Ever wonder why your mood sometimes sinks for no clear reason? It turns out, the answer might lie deep in your gut—literally. While most people know serotonin as the brain’s “feel-good” chemical, fewer realize that nearly 90% of it is made in the gut. Even more surprising? Your gut bacteria play a major role in how much serotonin your body can produce—thanks in part to a microbial metabolic route called the shikimate pathway. Let’s explore how your microbes may be influencing your mood from the inside out.
Serotonin is made primarily in the brain and the gut.
- Central Nervous System (Brain) in the Raphe nuclei in the brainstem neurons
Serotonin that is made in the brainstem is the true “feel-good” messenger. It plays a key role in lifting your mood, supporting deep sleep, calming pain, balancing appetite, regulating temperature, and sharpening focus. This is the serotonin that directly influences how you feel mentally and emotionally. But here’s the fascinating part, it has to be made right there in the brain, because serotonin can’t cross the blood-brain barrier. That means your body depends on the right building blocks (such as the amino acid tryptophan from meat, eggs, legumes) and signals to keep this internal mood engine running smoothly.
- Gastrointestinal Tract (Gut) mainly in the Enterochromaffin cells of the small intestine using tryptophan from food and from the microbiome in the large intestine via the shikimate pathway. 90–95% of total body serotonin is made in the gut.
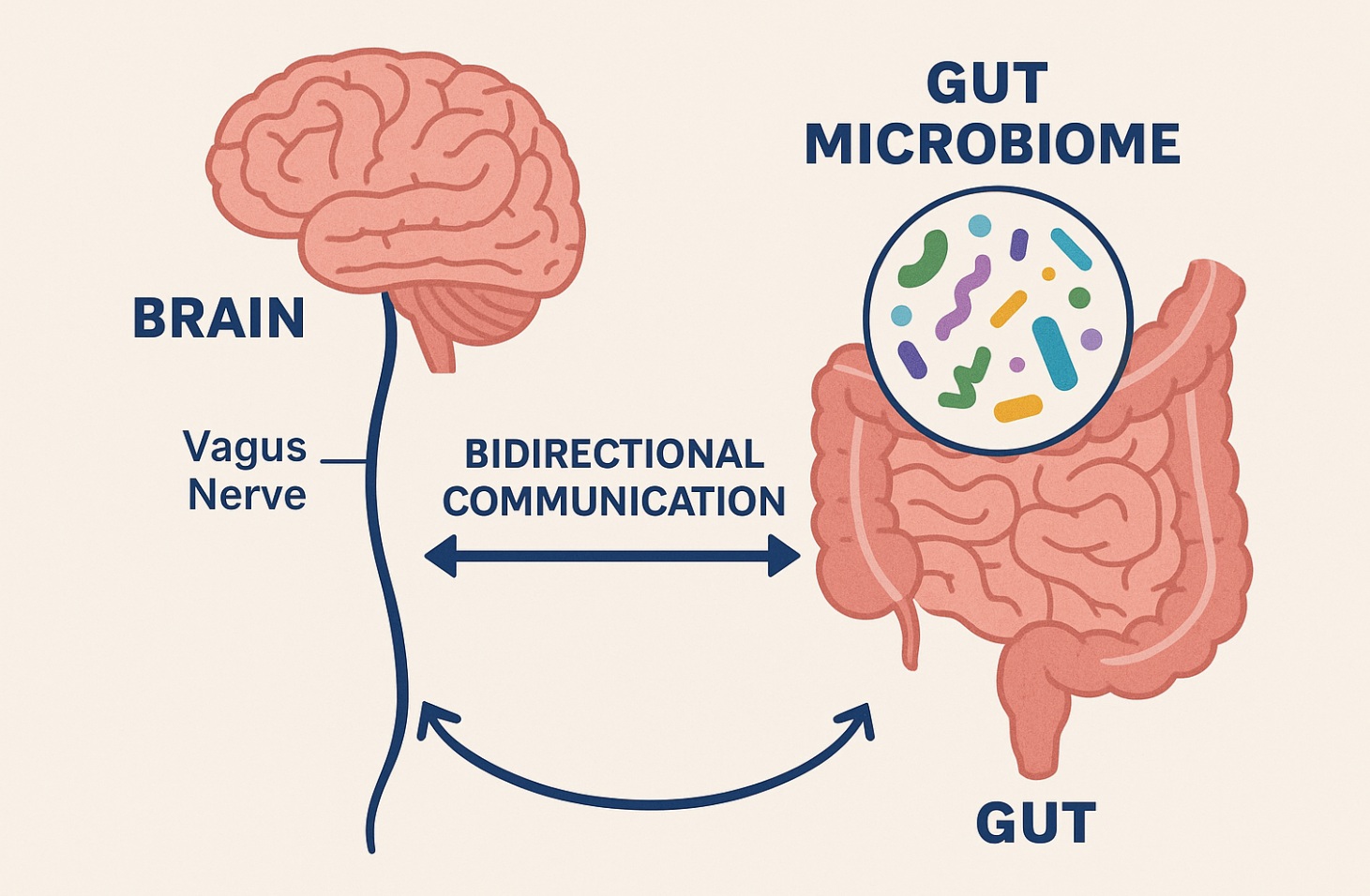
Serotonin in the gut does so much more than most people realize. While it doesn’t directly control your mood, it plays a powerful behind-the-scenes role—helping to keep your digestion smooth, your enzymes flowing, your body’s pain signals in check, and your immune system balanced. It also sends messages up to your brain through the vagus nerve, creating a strong gut-brain connection. In short, gut serotonin helps set the stage for how your body feels—and how your brain responds. I’ll explain more about how this works below.
Gut-brain axis
Here are a few concrete examples of how gut-derived serotonin (which doesn’t cross into the brain) can still influence mood and brain function indirectly via the gut-brain axis, vagus nerve, and immune signaling:
-
Vagus Nerve Activation is Brain Feedback
When gut serotonin levels rise (e.g., after a meal), it stimulates local enteric neurons which have a calming vagal feedback that can modulate anxiety and depression, even without serotonin entering the brain.
-
Serotonin Balances Our Immune Response
When gut serotonin interacts with immune cells in the intestinal wall (like dendritic cells and macrophages) it can trigger pro or anti inflammatory cytokine release. When the gut is chronically inflamed, serotonin triggers inflammatory cytokines which can cause anxiety and depression.
-
Microbiome Shape-Shifting via Serotonin To GABA=Calm
Some gut bacteria respond to serotonin levels by changing their gene expression and colonization behavior. For instance, serotonin can enhance the growth of spore-forming bacteria that produce metabolites like GABA that affect brain chemistry in a calming way, even without serotonin crossing the blood brain barrier.
-
Intestinal Serotonin Affects Pain and Sensory Processing
Intestinal serotonin plays a key role in how we sense and respond to digestive activity. When levels are balanced, digestion flows smoothly, gut sensations feel normal, and mood remains steady. But when serotonin is too high, it can lead to cramping, diarrhea, and heightened gut sensitivity. When we have too low serotonin, it can cause constipation, sluggish digestion, and a dull or disconnected feeling in both body and mind.
Microbiome: The Essential Support
Serotonin production is controlled partly by the health of the gut microbiome and the health of the gut in general. When the gut is healthy, you have a proper amount of good bacteria (Lacto, Bifido, etc), your lining is strong, you have a thick protective mucus layer and very little inflammation.
Some things that create an unhealthy gut:
- Infection
- Chronic stress, trauma
- Poor diet including processed foods or non-organic foods, lacking in whole fresh organic foods
- Toxin exposure
- Excessive alcohol use
When the gut lining is damaged becomes porous and weak. This allows particles of dead bacteria (LPS) into the blood which causes a major inflammatory reaction and higher levels of cytokines IL-6, IFNg, and TNFa. These circulating inflammatory cytokines cause a tryptophan shift from making serotonin to making IDO instead. IDO feeds the much needed immune functions that have been called into action by the cytokines. However, IDO then causes a higher amount of neurotoxins that directly cause depression and or anxiety.
In closing, understanding the microbiome’s influence on serotonin shifts how we think about depression. It’s not just a chemical imbalance in the brain, it may also be a microbial imbalance in the gut. Supporting beneficial bacteria, avoiding microbiome disruptors like glyphosate, and fueling the system with nutrient-dense, fiber-rich foods can be powerful tools in your mental health toolkit. The next time you’re feeling low, don’t just ask what’s going on in your head, ask what’s happening in your gut. If you have any questions please feel free to reach out using the link below.